What every architect needs to know about air and SarsCov2

Any infection control strategy can be compared to Swiss cheese. A single strategy is like a single barrier, full of holes. A number of slices of defences adds up towards a near blockage of transmission – they all need to be taken together. We will focus here on updating the language based on newer and more accurate science, and on adding Measurement, Ventilation and Filtration to the solutions that architects and engineers can play a role in implementing.
We have gone through a year of life with Covid-19, yet the pandemic appears to be only worsening. Worldwide deaths have exceeded two million, and few countries seem to have it under control. New variants are proving more transmissible, and are spreading faster than vaccination campaigns. Part of the reason for Ontario’s prolonged agony and tragedy is that we continue to treat Covid—now known to be an airborne pathogen—with the lesser precautions appropriate to droplet transmission.
At the most reductive level, architects design “volumes of air” that we live and work in. The purpose of this article is to appeal to Canadian architects and engineers to consider how architectural and engineering interventions can reduce the transmission of Covid, most notably through improved ventilation, filtration and airflow design. In effect, interventions like ventilation and filtration are the equivalent of providing PPE for physical spaces—and are especially important for places like classrooms and long term care facilities, where consistent physical distancing and mask-wearing are not always possible.
Thousands of experts in epidemiology, medicine, aerobiology, engineering and infection control have been urging Governments and the WHO to update their guidance and leadership (WHO has recently updated their guidance for LTC spaces here). As per a recent open letter from the Ontario Nurses’ Association:
…the Public Health Agency of Canada (PHAC) recognized on November 4, 2020 that SARS-CoV-2 is transmitted by fine aerosols, as well as larger respiratory droplets. PHAC’s position was updated to be consistent with an earlier change made by The Center for Disease Control and Prevention (CDC) on October 5, 2020, which recognized that COVID-19 can be spread by airborne transmission, through exposure to virus in small droplets and particles that can linger in the air for minutes to hours. As well, the World Health Organization (WHO) has updated its guidance to include transmission via aerosols.
Public Health Ontario (PHO) and other provincial governments need to reconsider their stance on airborne transmission. A number of recent studies, including this review article from the Journal of Hospital Infection, unpack the issue and provide clear guidance as we move into a second year of lockdowns and restrictions on social activities.
Part of the conclusion of the Journal of Hospital Infection’s article states:
What does [treating SarsCov2 as airborne] mean for infection control practitioners in healthcare, as well as the general population? Aside from the obvious benefits of Personal Protective Equipment (PPE), the existing evidence is sufficiently strong to warrant engineering controls targeting airborne transmission as part of an overall strategy to limit the infection risk indoors. These would include sufficient and effective ventilation, possibly enhanced by particle filtration and air disinfection; and the avoidance of systems that recirculate or mix air. Opening windows, subject to thermal comfort and security, provides more than a gesture towards reducing the risk of infection from lingering viral particles. Measures to control overcrowding in both healthcare and confined indoor environments in the community, including public transport, are also relevant. There exist a range of cost-effective measures aimed at diluting infectious airborne particles in homes and hospitals that are easily implemented, without major renovation or expenditure. These will serve to protect all of us as we seek the evidence required to further reduce the risk from Covid-19 over the coming months and years. It is time to discard the myths and rewrite the science of viral transmission.
Architects and engineers can and should take a leading role, since our self-regulating professions are committed to serving the public interest. When we are made aware of how the spaces we design can influence the transmission of SarsCov2, we are obliged to act on that information by providing both leadership and solutions.
Architects and allied professionals can readily obtain the tools needed to assess and mitigate transmission of Covid through Indoor Air Quality (IAQ) measuring, ventilation, filtration and controls. We can—and have—taken a leading role in advising our Provincial government on how the transmission of Covid must be addressed in the design and retrofit of long-term care and healthcare environments. We must also do the same concerning schools, MURBs and other residences. The Ontario Society of Professional Engineers has taken just this kind of leadership with their recent public statement.
It reads, in part:
OSPE believes that airborne transmission is one of the main reasons why we are seeing so many outbreaks in schools and long-term care facilities across the province. With outdoor temperatures dropping, many of these buildings have shut themselves off from fresh air that would have helped get rid of these COVID aerosol particles. Instead, many of these buildings have closed HVAC systems that recirculate the same, potentially infected, air.
While we could get right into the weeds with science and guidance, I would first point the reader to (1) four (2) critically (3) important (4) resources that support the argument that we need to declare SarsCov2 as an airborne pathogen, which can be reviewed in full when time permits.
It should be noted that none of these recommendations negate or supercede any other public health directives or measures, but rather enhance these with ventilation considerations. SarsCov2 transmission risks can be mapped on a matrix of measures, with increasing/decreasing risk according to the measures taken. Ventilation is one of these considerations. This is most easily described by the British Medical Journal’s image below [adapted with icons from The Noun Project]:
As lawyer Jonathan Mesiano-Crookston notes:
[The historical] discussion of “close contact” primarily driving infection led to the six feet that we have seen today called a “safe distance.” It was indirectly supported by a few early studies where people tried to colonize bacteria from sneezes, but could not do so outside this “close contact” distance, although studies concluding the contrary seemed to be ignored.
Overall, despite the strong evidence to the contrary, the myth that respiratory illnesses are transmitted by respiratory droplets which are ejected from sick people and land on recipients has persisted, despite not being conclusively proven by any study.
That said, most transmission of course does occur within closer quarters, as [Charles V.] Chapin correctly identified in his 1910 book—but this is explained by higher concentrations of aerosols at those distances, and does not limit the transmission to droplets.
As the Journal of Hospital Infection article summarizes:
There is little, if any, direct evidence for transmission of SARS-CoV-2 via any specific pathway. This statement applies to fomites and direct contact just as much as for large droplets and smaller airborne particles. It is notable that transmission through large droplets has never been directly demonstrated for any respiratory virus infection.
Moreover, in seeking to limit the transmission of Covid and future viruses, the precautionary principle dictates that we should consider coronaviruses as airborne unless proven otherwise. For architects and engineers, air quality is within our bailiwick, and we need to pay attention to airflow, volumes, airtightness, ventilation and filtration for a whole host of reasons—including, urgently, the current pandemic emergency.
Thermal Energy Design and Air Quality in Buildings
Since the 1970s, demands for energy efficiency—and now, net-zero and zero-carbon emission design—have sought to control heat loss through a range of envelope and ventilation strategies. The first approach consisted of making airtight buildings, which limited heat loss, but then led to a buildup of CO2, indoor air pollutants and humidity, also known as Sick Building Syndrome (SBS).
The second step, in the 1980s was to introduce controlled ventilation systems, often with heat recovery (HRV/ERV). In larger buildings Dedicated Outdoor Air Systems (DOAS) usually included heat recovery cores and filters. This resulted in indoor air being purged of CO2, achieving a balanced humidity (30-50% RH) and having reduced levels of pollens and other pollutants. MERV and HEPA filters further reduced pollutants, including mould and viruses.
While HRVs are now mandatory in new construction, most homes predating 2017 (including my own) do not have these systems. Incidentally, the onset of SBS begins at 800ppm of CO2 as measured in indoor spaces. Health Canada has suggested an upper limit of 1,000ppm, however the best practice is to aim for the closest approximation of outdoor air concentrations (~450ppm) with integral heat-recovery to limit energy waste.
The problem of Legacy Buildings
New buildings are easy—we can design a ventilation strategy with filtration and heat recovery, and we can measure its performance through real-time CO2 levels and other indicators. But with existing building stock, we may not even have a ventilation system in place. Since we have inherited a wide range of buildings from every era of design and engineering, we must also have a strategy for determining and then addressing air quality issues in our legacy buildings—whether they be homes, schools, offices or healthcare spaces. We propose the framework of Measure, Ventilate and Filter, in that order.
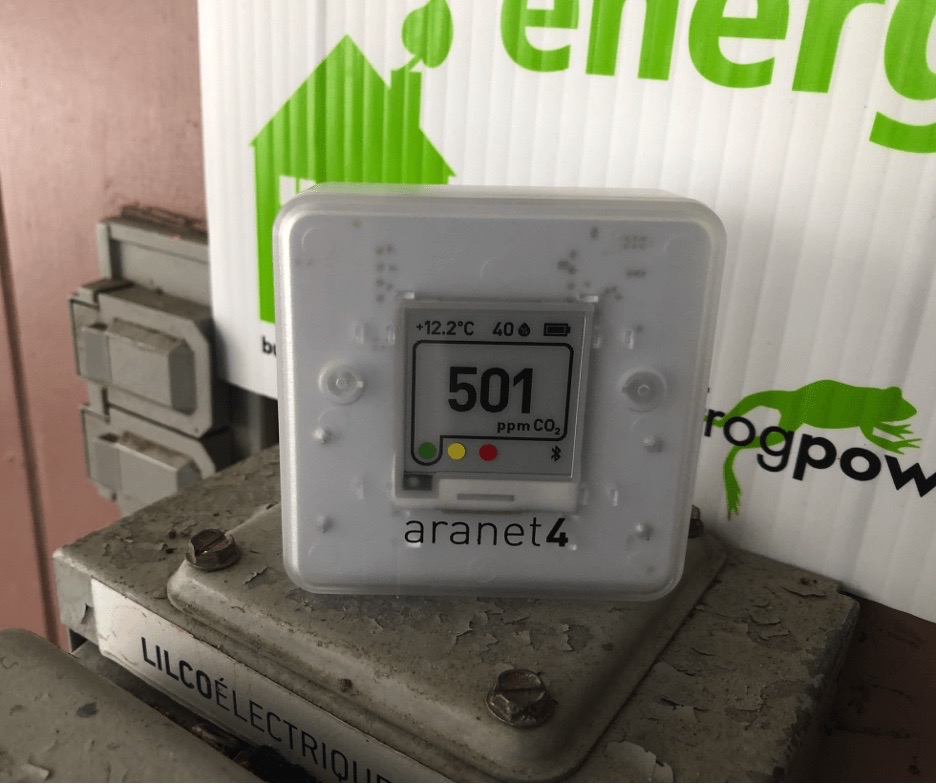

Here is one example: As I write this, my own office measures 1445ppm of CO2. That corresponds to a re-breathed fraction of air of roughly 2.7%. I can see that the outdoor air’s CO2 levels are currently at 501ppm. My goal should be to get my office air as close as possible to the outdoor levels, but I would be happy with around 700ppm of CO2. Whoever built this place did not even put a ventilation fan in the bathroom, or the kitchen! So I open a window, and within 10 minutes, the monitor on my desk drops down to 1053ppm – better. If the CO2 does not lower, this could be due to airflow. For example, if air from a higher occupancy area in the house is now equalizing through the room I am in, I may be inadvertently exposing myself—now sitting in the pathway of this exciting airflow—to a higher level of risk. Smoke pencils and other tools can highlight airflow in these cases, which is why it is important to work with professionals whenever possible—and especially when the concern is a space for a group, care home, healthcare or other public occupancy.
But now it is getting cold in my office—should I crank my thermostat to bring it up to a comfortable level? I could, but I am only occupying one room in my house, so I can close my door, put on a sweater and toque, and switch on the radiant ceramic heater beside my workstation. As my Aranet4 CO2 monitor updates itself every five minutes, I can adjust the window from wide open to about 1/2″—which over time it seems is enough to keep this one room of the house under 1,000 ppm of CO2—not the best, but pretty decent for this older house.
Fresh air, check. Thermal comfort, check. Now, while I am isolated at home and at zero risk of receiving Covid-19 from any office colleagues, it would be foolish to leave my window wide open for disease prevention. But I think sharper and design faster when my mind is as clear as the air that I breathe, so simply put, I prefer it this way. (Numerous studies indicate cognitive impairment correlated to rising CO2.)
- 420ppm – Fresh outdoor air
- 420-800ppm – optimal air quality indoors
- 1000ppm – brain cognitive function decreases by 15%
- 1400ppm – brain cognitive function decreases by 50%
The next step would be to improve my whole building-level filtration by checking to see that my furnace filter has a new minimum-level MERV or HEPA filter installed. Ideally, if I shared my office with anyone else, I would also be masking, distancing and filtering local air with a portable unit, such as the JASPR HEPA device I have been testing.
At home, my localized HEPA filter has its own PM2.5 monitor, which in the image above just spiked because we were cooking. When this happens, the ECM motor will quickly ramp up to top speed to clear the air of these particulates within about 10 minutes.
But what if I am in a shared office? How can I work safely with others in the same room? What about higher-risk, longer-duration indoor activities, such as lunchrooms in a hospital (unmasked, talking), or classrooms in a school? The same principles apply: measure first, then ventilate (checking airflow where possible), then filter–centrally and locally.
These measures should be taken in addition to recommended public health measures. Measuring, ventilation, and filtering solutions can be scaled to commercial indoor environments and classrooms, following Health Canada guidelines for unit types and observing airflows so as to limit lateral mixing.
Measure First
While I am not recommending architects step outside of their area of expertise, anyone (including architects) can educate themselves on IAQ/EAQ and purchase measuring devices to test their own homes, and potentially their clients’ homes, and then share the results with their professional engineering colleagues to help develop solutions with them—just as we do in our professional practice. People produce CO2 when they exhale, and CO2 can be accurately measured with a low-cost sensor.
For about $300, a portable CO2 monitor provides an instant readout of CO2 in any space, be it a bus, car, school, hospital, classroom or bedroom. I like the Aranet4 because after calibration, it has low power draw, samples every 5 minutes and is essentially always on. It logs data on a smartphone app via bluetooth or wireless.

There is a wide range of consumer- and professional-grade air quality measuring systems in the marketplace. At home, I also use a building-integrated device called Airthings that provides data on CO2, temperature, humidity, radon, PM2.5 and barometric pressure that feeds into a dashboard app.
As a best practice, the renovated OAA headquarters in Toronto is using the Airthings system, which verifies that CO2 levels are always within accepted norms. The building’s deep energy retrofit incorporated a 100% fresh air system with filtration and heat recovery. This system even uncovered an issue with low humidity (20%) that would not have been discovered otherwise, and that is subsequently being addressed.
In all new commercial projects, we ask our M&E consultants to control DOAS and ERV/HRV units by CO2 sensors—which adds a marginal increase in cost, but provides significant benefits and additional energy savings when spaces have low or zero occupancy and CO2 is not produced in the spaces.
To keep it simple, we can look to CO2 as a proxy gas for a wide range of other issues: from the risk of indoor airborne infection, to air changes per hour, to occupancy, to ‘Rebreathed Air Correlations’ (chart below). We can also use CO2 levels as a general indicator of Indoor Air Quality (IAQ). The closer indoor air comes to outdoor levels of CO2, typically the lower the TVOC, radon and PM2.5 levels.
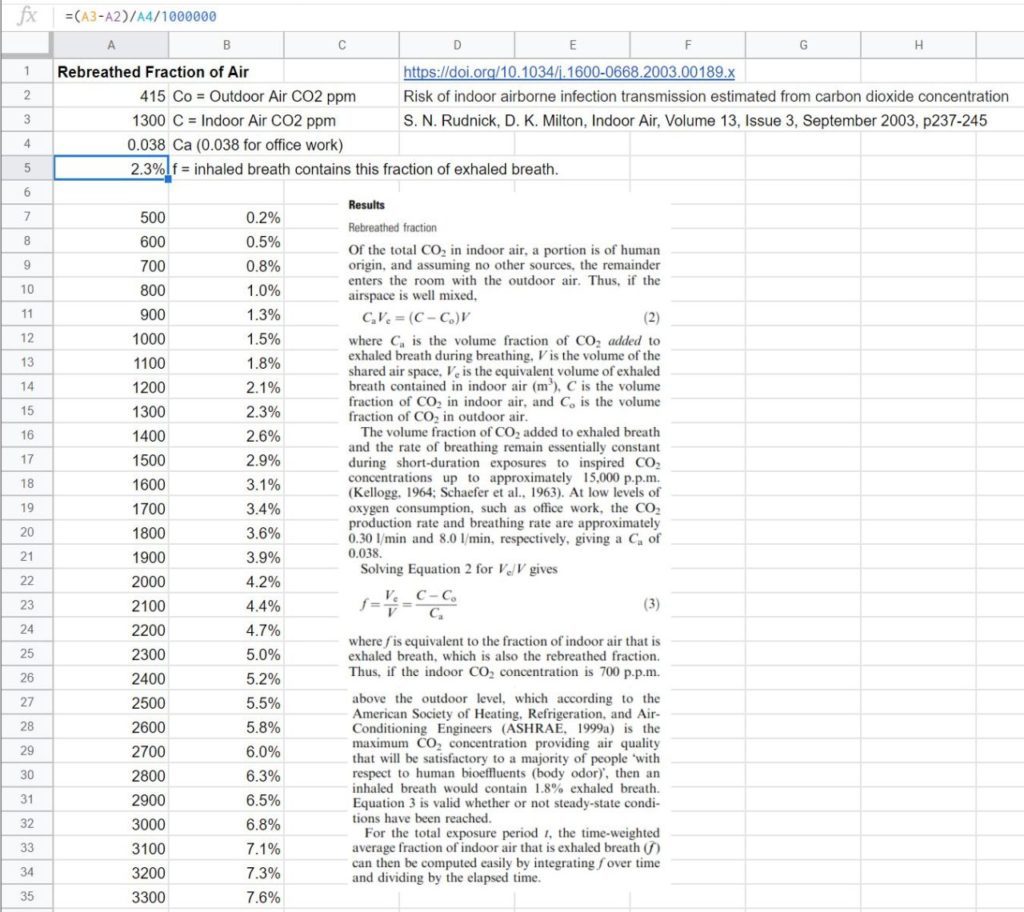 Source: https://onlinelibrary.wiley.com/doi/abs/10.1034/j.1600-0668.2003.00189.x and https://pubmed.ncbi.nlm.nih.gov/12950586/
Source: https://onlinelibrary.wiley.com/doi/abs/10.1034/j.1600-0668.2003.00189.x and https://pubmed.ncbi.nlm.nih.gov/12950586/
Ventilation and filtration
Once we have measured the quality of indoor air in a given space, thus establishing a baseline to improve upon, then we can undertake a range of strategies for mitigating air quality issues. Many of these can also reduce the transmission and persistence of the SarsCov2 virus in airborne aerosols and droplets. Post-intervention follow-up with subsequent measurements can confirm whether our strategy has been effective. To simplify even further, many HEPA units even have displays built in with IAQ metrics of one form or another. Public Health Ontario has also issued guidelines or portable ventilation units.

In order to assure proper air changes for a specific occupancy, professionals can refer to their own guidance documents, but Public Health Canada’s recent guide on indoor ventilation during the pandemic can be a starting place.
While measuring CO2 can help describe the difference between indoor and outdoor air quality, it can similarly provide a benchmark for Air Changes per Hour (ACH). An ACH of 3 is recommended at a minimum to help reduce SarsCov2 transmission, with an ACH of 6 being recommended for congregate environments such as long-term care homes, schools and healthcare environments.
Educate, Measure, Ventilate and Filter
Architects are at the front end of the design, renovation and remediation of almost every public building. To that end, we urgently need to consider IAQ measures in the design of buildings—both in terms of the materials we use, the envelopes we design, but also the measurement and control of air in the systems that we coordinate through our professional engineer colleagues. Accepting the correct terminology and definitions of Airborne Transmission of SarsCov2 is a critical first step in identifying causes and developing solutions.
We can then proceed with three critical steps in using design to improve air quality and decrease the risk of transmission of coronavirus in buildings:
- Measure: It is now easier than ever to measure humidity, CO2, PM2.5 and radon, and subsequently to design systems that bring air quality to be within the range of accepted values, as provided by public health agencies and professional standards.
- Ventilation (with heat recovery where possible): As professionals trained in the science of thermodynamics, we are also obliged to consider the public health benefits of not only energy performance and carbon mitigation, but also Indoor Air Quality (IAQ). Any building with a properly designed air tight envelope and heat recovery system will also bring the benefits of a draft-free and healthy home. This comes with co-benefits of increased durability, balanced humidity and lower operating costs.
- Filtration:In instances where there is inadequate capacity for improved ventilation, a strategy of filtering recirculated indoor air should be taken as a less effective but nevertheless important way to improve IAQ and remove infectious airborne particles. Filtration can be central (ie. furnace and/or HRV filters) and local (room by room). Filtration can be thought of like PPE for buildings. We can work to develop solutions to isolate airborne transmission by use of filters, with or without ventilation strategies, even though ventilation is of greater importance.
Architects are developing expertise in physical design for distancing, and the design of ever more airtight structures with complementary natural and mechanical ventilation strategies for 100 percent fresh air. In tandem, we can also learn to measure IAQ with a range of readily available devices, and we can test spaces to see whether the buildings we have designed are within the suggested ranges of these measures. Where IAQ can be improved, we can recommend a strategy of ventilation and filtration together with our engineering consultants. We can also provide guidance and leadership to our provincial governments, in instances where well-considered measurement, ventilation and filtration strategies should be implemented in a systemic manner.
This article was adapted and excerpted from a blog post by architect Andy Thomson, which can be found in its full version here. Andy Thomson was a former HRAI-certified HVAC/HRV designer/installer and trained as a R2000 program delivery agent, and has personally installed and balanced thousands of HRVs and performed as many blower-door tests. Since that time, he has been involved in IAQ research & measurement for clients with MCS (Multiple Chemical Sensitivities) and in the review and testing of IAQ measuring & monitoring equipment. As a member of the OAA Building Committee, he was responsible for the installation of the Airthings system at the OAA HQ, which Thomson Architecture uses on most of its projects.
Disclaimer: Thomson Architecture, Inc. has used reasonable efforts to provide accurate and current information in this article, but we cannot accept any liability for the content and we make no warranty or representation of any kind concerning the accuracy or suitability of the information contained on this website for any purpose. We also provide links to other websites as a convenience but not as an endorsement. You should never rely on, or take, or fail to take any action, based upon the information on this website alone without independent verification. Readers should obtain appropriate legal and technical advice. The information presented here is for educational and information purposes only, which you may use at your own risk.
References:
- WHO Adequate Ventilation revised January 8, 2021 (page 7): https://apps.who.int/iris/bitstream/handle/10665/338481/WHO-2019-nCoV-IPC_long_term_care-2021.1-eng.pdf
- https://www.journalofhospitalinfection.com/article/S0195-6701(21)00007-4/fulltext
- https://ricochet.media/en/3423/there-is-still-time-to-address-aerosol-transmission-of-covid-19
- https://docs.google.com/document/d/1fB5pysccOHvxphpTmCG_TGdytavMmc1cUumn8m0pwzo/edit
- https://ospe.on.ca/featured/engineers-call-on-ontario-to-refocus-efforts-on-the-airborne-transmission-of-covid-19/
- https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/guidance-documents/guide-indoor-ventilation-covid-19-pandemic.html
- https://www.canada.ca/en/health-canada/programs/consultation-residential-indoor-air-quality-guidelines-carbon-dioxide/document.html
- https://coronavirus.jhu.edu/map.html
- CSA Z317.2:19, Special requirements for heating, ventilation, and air-conditioning (HVAC) systems in health care facilities
- CSA Z8002:19, Operation and maintenance of health care facilities
- http://www.health.gov.on.ca/en/public/programs/ltc/docs/home_design_manual.pdf
- https://dash.harvard.edu/bitstream/handle/1/27662232/4892924.pdf?sequence=1
- Australia infographics on the Anatomy of outbreaks (closed, indoors, airborne transmission) https://www.abc.net.au/news/2021-01-25/covid-19-spread-through-australia-over-year/13078574?nw=0
- Open letter from ONA, January 25, 2021: https://www.ona.org/news-posts/open-letter-airborne/
- VIDEO: https://www.pbs.org/newshour/show/how-to-protect-yourself-from-the-new-coronavirus-strains
- Re-useable PPE: https://www.cdc.gov/coronavirus/2019-ncov/hcp/elastomeric-respirators-strategy/index.html
- Calculating Viral Risk as a function of CO2: https://pubmed.ncbi.nlm.nih.gov/12950586/
- ABC Radio Australia, the ‘A’ word: https://www.abc.net.au/radio/melbourne/programs/mornings/kim-prather-covid-aerosols/13135544
- https://www.nature.com/articles/d41586-021-00251-4
- https://www.toronto.com/news-story/10313852–evidence-is-now-overwhelming-3-things-to-know-about-airborne-covid-19/
- https://www.washingtonpost.com/health/2021/02/10/carbon-dioxide-device-coronavirus/
- https://youtu.be/OQ6DhgwgtGw Interview w. Dr. Joseph Allen of the Harvard School of Public Health on Healthy Buildings, IAQ, Covid, etc.
- WHO (finally) has updated their guidance to include ventilation: https://apps.who.int/iris/handle/10665/339857

